Non-fatal strangulation and its link to brain injury
WARNING: This article discusses domestic and family violence and may be distressing for some readers.
Non-fatal strangulation is a dangerous, yet often overlooked, form of domestic and family violence (DFV) that poses severe and lasting risks to survivors. Although it can leave no visible marks, the harm inflicted by non-fatal strangulation can have long-lasting effects, including a brain injury due to a lack of oxygen reaching the brain.
Understanding non-fatal strangulation
Strangulation occurs when pressure is applied to the neck, obstructing airflow or blood flow to the brain. This pressure can be applied with one or both hands, a collar, rope, clothing, or by using other body parts to put pressure on the neck. Even brief periods of oxygen deprivation can lead to a hypoxic brain injury. Strangulation is a commonly used by perpetrators of domestic and family violence to assert power and control over someone.
Key statistics:

Despite these alarming statistics, strangulation is often underreported and under-recognised by healthcare professionals, police, and social services.
Synapse advocates for individuals who have presented to police and medical staff who have experienced non-fatal strangulation to be screened for brain injury.
It’s important to note that both men and women can experience non-fatal strangulation.
How a brain injury occurs
Non-fatal strangulation can cause a brain injury as it can cut off oxygen and blood flow to the brain. For the brain to function properly it needs both blood flow and oxygen. While it might not be immediately obvious, this can lead to a traumatic brain injury.
It doesn’t take much time or force for a brain injury to occur. When your brain is deprived of oxygen for less than a minute, it can begin to affect the brain.
Symptoms may not be immediate, but survivors may later experience:
- Memory problems
- Difficulty concentrating
- Fatigue
- Mood swings or emotional instability
- Persistent headaches
- Loss of coordination.
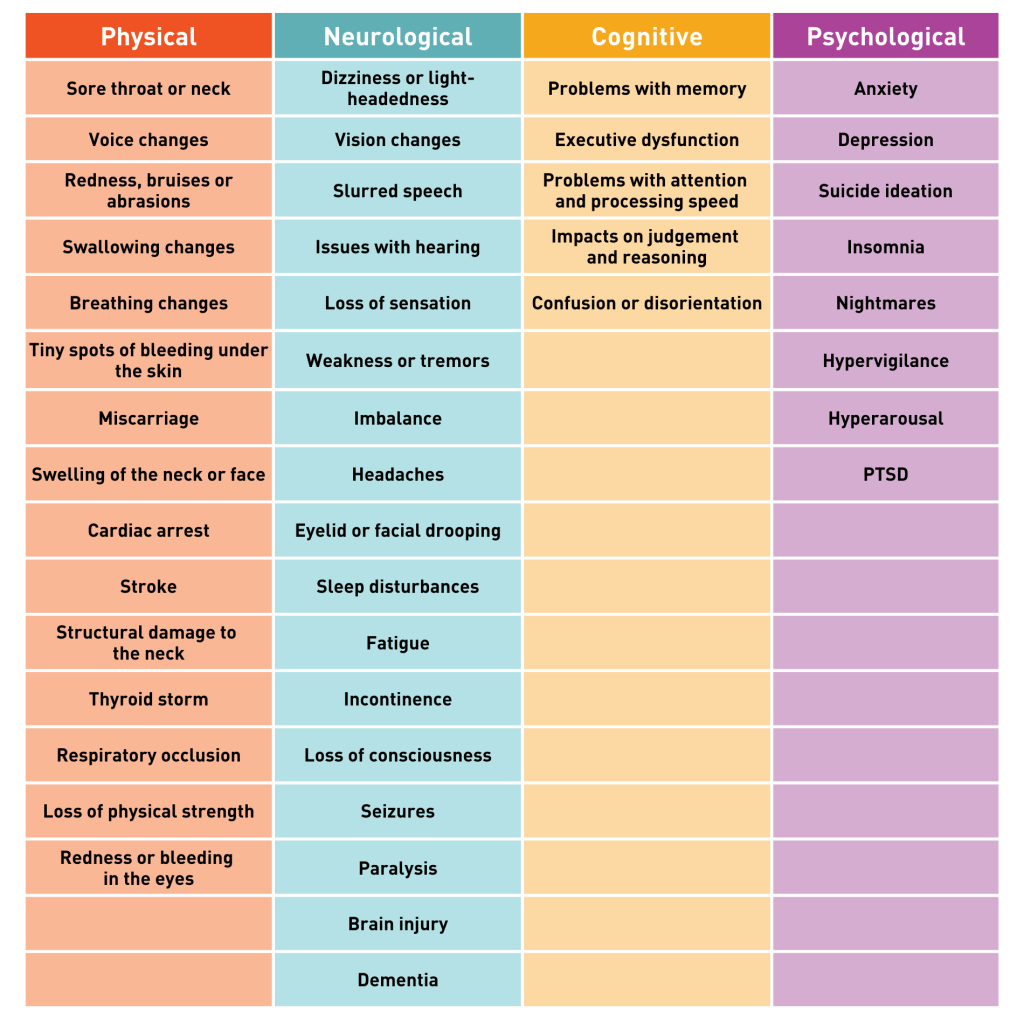
The table below breaks down the full list of physical, neurological, cognitive, and psychological symptoms people may experience after non-fatal strangulation.
Learn more about anoxic and hypoxic brain injury with our fact sheet.
Why screening and awareness are both critical
Non-fatal strangulation can easily go undetected due to the lack of visible injuries or the delay in symptoms, as they often emerge gradually after the abuse. We don’t have the full picture of how many individuals are impacted by non-fatal strangulation, due to a lack of reporting and the reluctancy to seek help or medical support.
Many healthcare providers, police, and support services lack the appropriate training to recognise, screen for, and address possible brain injuries resulting from strangulation.
Challenges often include:
- Misdiagnosing symptoms attributing them to psychological distress or unrelated health issues.
- Survivors being unaware that their symptoms may be linked to brain injury.
- Lack of routine screening for brain injuries in domestic and family violence cases.
A consultation paper by the Queensland Law Reform Commission found that survivors who reported their strangulation experience to police felt that complaints were sometimes minimised, dismissed, or disbelieved. Some survivors felt that police treated them differently because they were Aboriginal or had a culturally and linguistically diverse background. While medical professionals supported the survivors, more than police, the commission report found that there was not enough understanding of strangulation and its ongoing impact.
Recommendations for improving detection and support
- Implement routine screening: Incorporating a brain injury screen into all domestic and family violence assessments, especially when strangulation is reported or suspected.
- Training professionals: Educating medical professionals, police, social workers, and legal professionals to recognise the signs of a brain injury.
- Providing targeted support: Ensuring survivors have access to medical assessments, rehabilitation, and trauma-informed care.
- Men’s behaviour change programs for offenders: Include a brain injury screen in behaviour change programs to reduce recidivism and support positive rehabilitation outcomes.
Non-fatal strangulation is a silent epidemic that demands urgent attention. By raising awareness, improving screening processes, and providing specialised support – we can better protect survivors from the devastating impacts of a brain injury.
Synapse is committed to advocating for those affected by family and domestic violence and promoting evidence-based practices that ensure every survivor receives the care they deserve.
Sources:
- Family, domestic and sexual violence (Accessed April 2025): https://www.aihw.gov.au/family-domestic-and-sexual-violence/responses-and-outcomes/health-outcomes
- Non-fatal strangulation: A highly lethal form of gendered violence (Accessed April 2025): https://noviolence.org.au/wp-content/uploads/2022/08/Integrated-Lit-Review-NFS-FV-23.08.22.pdf
- Non-fatal strangulation is an important risk factor for homicide of women (Accessed April 2025): https://pmc.ncbi.nlm.nih.gov/articles/PMC2573025/
- Review article: Non-fatal strangulation: Hidden injuries, hidden risks (Accessed April 2025): https://dora.health.qld.gov.au/qldresearchjspui/bitstream/1/5529/1/Boos-2019-Emergency_Medicine_Australasia.pdf
- Strangulation: assessment following non-fatal strangulation in the context of an alleged assault (see strangulation documentation proforma) (Accessed April 2025): https://cdn.wchn.sa.gov.au/downloads/WCHN/womens-health/Strangulation_Assessment.pdf
- Time is of the essence: Domestic and family violence and the potential for acquired brain injuries in victim/survivors. NSW Health Education Centre Against Violence. (Accessed April 2025): https://www.ecav.health.nsw.gov.au/ArticleDocuments/3753/DFV_and_the_Potential_for_Acquired_Brain_Injury_Roundtable_Report_October.pdf.aspx
- Women’s stories of non-fatal strangulation: Informing the criminal justice response (Accessed April 2025): https://www.researchgate.net/publication/343620273_Women’s_stories_of_non-fatal_strangulation_Informing_the_criminal_justice_response